Deep learning in Radiotherapy
Imaging is crucial for the preparation of radiotherapy. A patient that is going to be irradiated undergoes multiple imaging sessions to prepare the treatment and during the treatment. These images are processed, interpreted and manipulated by various users such as radiation oncologists, radiographers, etc. To facilitate image processing and, ideally, automatize the workflow, we are developing deep learning-based solutions aiming at reduce human efforts and support tailoring the treatment for each patient.
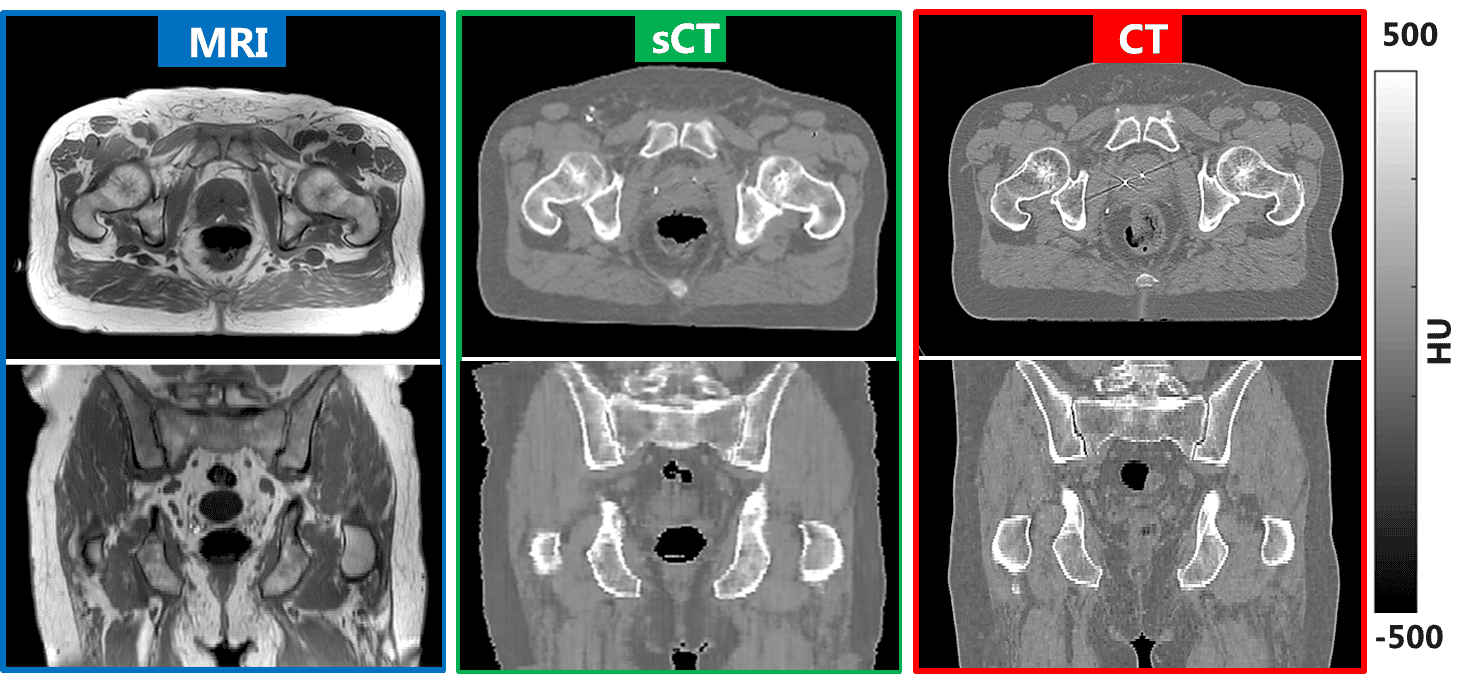
Synthetic-CT generation Computed tomography (CT) is the reference modality that enables planning of the irradiaiton to target the tumour and spare the surrounding healthy tissues. Along with CT, magnetic resonance imaging (MRI) facilitates with its superior soft tissue contrast the localization and delineation of tumor and other clinially relevant structures. In this theme we are working on using convolutional neural networs to derive synthetic-CT from MRI thereby eliminating CT leading to an MRI-only simulation workflow. In this way, the patient does not have to undergo a CT exam anymore and the problematic registration between CT and MRI can be eliminated. Currently, our work has helped to introduce MRI only planning in our clinic for prostate and rectum cancer patients validating commercial solutions. In addition, we are developing synthetic-CTs for more challenging sites such as pediatric, brain and lung radiotherapy patients.
Related work
- Maspero M, Savenije MHF, Dinkla AM, Seevinck PR, Intven MPW, Jurgenliemk-Schulz IM, Kerkmeijer LGW, van den Berg CAT. Dose evaluation of fast synthetic-CT generation using a generative adversarial network for general pelvis MR-only radiotherapy. Phys Med Biol. 2018 Sep 10;63(18):185001.
- Maspero M, Bentvelzen LG, Savenije MHF, Guerreiro F, Seravalli E, Janssens GO, van den Berg CAT, Philippens MEP. Deep learning-based synthetic CT generation for paediatric brain MR-only photon and proton radiotherapy. Radiother Oncol. 2020; 153:197-204.
- Dinkla AM, Wolterink JM, Maspero M, Savenije MHF, Verhoeff JJC, Seravalli E, Išgum I, Seevinck PR, van den Berg CAT. MR-Only Brain Radiation Therapy: Dosimetric Evaluation of Synthetic CTs Generated by a Dilated Convolutional Neural Network. Int J Radiat Oncol Biol Phys. 2018; 102(4):801-812.
- Spadea MF & Maspero M, Zaffino P, Seco J. Deep learning based synthetic‐CT generation in radiotherapy and PET: A review. Med Phys. 2021;48(11), 6537-6566.
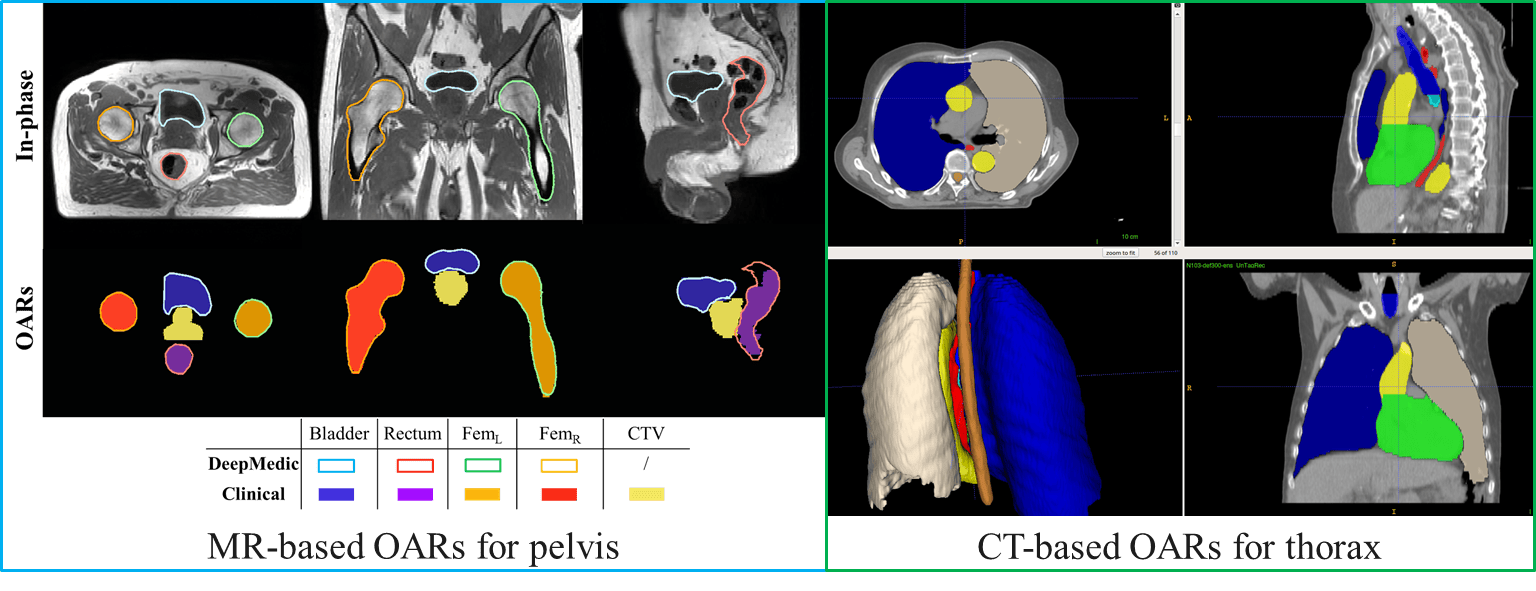
Automatic contouring and registration Deep learning can streamline image post-processing. Currently, image registration and contouring can require considerable manual interaction, e.g. a radiographers spend on average 1 hour per patient on image processing. In total, this accumulates to a significant number of yearly men hours where personnel shortage is severe. We have developed in collaboration with computer scientists and medical physicists of the radiotherapy department several deep learning solutions that are now used clinically for automatic delineation of organs-at-risks for pelvis, lung, esophagus, abdomen, thorax, head and neck and pediatric patients both MRI and CT-based. Solutions for other anatomical sites and imaging modality are under development.
Related work
- Savenije MHF & Maspero M, Sikkes GG, van der Voort van Zyp JRN, T J Kotte AN, Bol GH, T van den Berg CA. Clinical implementation of MRI-based organs-at-risk auto-segmentation with convolutional networks for prostate radiotherapy. Radiat Oncol. 2020;15(1):104.
Adaptive cone-beam guided radiotherapy Cone-beam CT (CBCT) is being employed on the linear accelerators to guide patient positioning prior to irradiation. Currently, the image quality of CBCT is sub-optimal due to various hardware and reconstruction issues. The goal of this research theme is to use deep learning to improve the quality of CBCT bringing it on-par with standard CT. This would enable new adaptive treatment schemes, where a treatment plan can be devised based on the daily patient anatomy minimizing target margins and dose to healthy neighboring tissue.
Related work
- Maspero M, Houweling AC, Savenije MHF, van Heijst TCF, Verhoeff JJC, Kotte ANTJ, van den Berg CAT. A single neural network for cone-beam computed tomography-based radiotherapy of head-and-neck, lung and breast cancer. Phys Imaging Radiat Oncol. 2020; 14:24-31.
- Kurz C, Maspero M, Savenije MHF, Landry G, Kamp F, Pinto M, Li M, Parodi K, Belka C, van den Berg CAT. CBCT correction using a cycle-consistent generative adversarial network and unpaired training to enable photon and proton dose calculation. Phys Med Biol. 2019;64(22):225004.
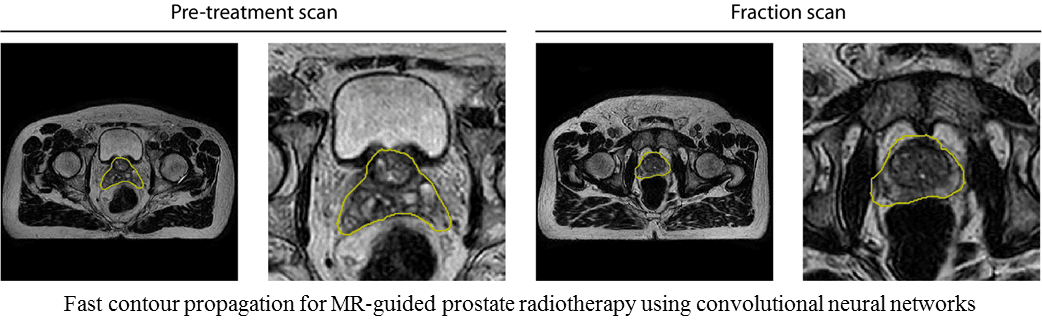
Adaptive MR-guided radiotherapy The introduction of online adaptive MRI-guided radiotherapy using the Elekta Unity MRI-Linac system pioneered at the UMC Utrecht, sets the time constraints for treatment adaptation even more stringent. While the patient is lying on the treatment contouring of targets and organs-at-risks should be performed in a minimum amount of time. The development of fast deep Learning solutions for auto-contouring, registration, image reconstruction, motion estimation and contour-propagation is essential to facilitate shorter treatment fractions.
Related work
- Eppenhof KAJ, Maspero M, Savenije MHF, de Boer JCJ, van der Voort van Zyp JRN, Raaymakers BW, Raaijmakers AJE, Veta M, van den Berg CAT, Pluim JPW. Fast contour propagation for MR-guided prostate radiotherapy using convolutional neural networks. Med Phys. 2020 Mar;47(3):1238-1248.
- Terpstra ML, Maspero M, d’Agata F, Stemkens B, Intven MP, Lagendijk JJ, van den Berg CAT, Tijssen, RH. Deep learning-based image reconstruction and motion estimation from undersampled radial k-space for real-time MRI-guided radiotherapy. Phys Med Biol. 2020;65(15):155015.
- Terpstra ML, Maspero M, Bruijnen T, Verhoeff JJ, Lagendijk JJ, van den Berg CAT. Real‐time 3D motion estimation from undersampled MRI using multi‐resolution neural networks. Med Phys. 2021;48(11):6597-6613.
- Terpstra ML, Maspero M, Sbrizzi A, van den Berg CAT. ⊥-loss: a symmetric loss function for magnetic resonance imaging reconstruction and image registration with deep learning. Medical Image Analysis. 2022, 102509.
Education on Deep learning in Radiotherapy Since 2019 we are organizing yearly a popular workshop on deep learning in radiotherapy focusing on principles and applications of deep learning in radiotherapy. Check out www.DLinRT.org for more informations.